Written by Briana Ondatje, ASU PhD Candidate in Neuroscience
It flashed across my screen in what seemed like a blaze of glory “Huntington’s disease treated for the first time”. The BBC reporting on a new therapeutic strategy out of the UK for Huntington’s patients. There is nothing quite like the excitement of having cracked at least part of a code that we as a research community have been working on for decades. I also had a similar feeling in 2023 when the drug, Qalsody, was approved by the FDA for the treatment of amyotrophic lateral sclerosis (ALS) for patients whose disease is caused by a genetic mutation in the gene SOD1. In recent years, there have been many exciting advancements in therapies for neurodegenerative disorders, including Alzheimer’s Disease (AD) and Parkinson’s Disease (PD), in addition to these advances for ALS and HD.
In a time when we are living longer, it is difficult to find someone who has not been impacted by a neurodegenerative disease. From family members to friends, many people experience the impact of neurodegeneration including AD, PD, HD, multiple sclerosis, ALS, frontotemporal dementia (FTD), Lewy body dementia and many others. Growing up, I witnessed my great-grandmother suffer from PD, which included losing her ability to form facial expressions, as well as most of her ability to verbally communicate. Despite her physical challenges, her mind remained, and I will never forget her eyes lighting up in recognition of me and saying my name upon walking into her home. I also witnessed the slow decline of my grandmother as she suffered with AD. I observed the peculiar way the disease affected her mind as she recognized both myself and my cousin as her granddaughters, yet she still felt compelled to introduce us to each other at my high school graduation dinner. While these are now family stories that incite fond memories, these are also the stories that inspire my future.
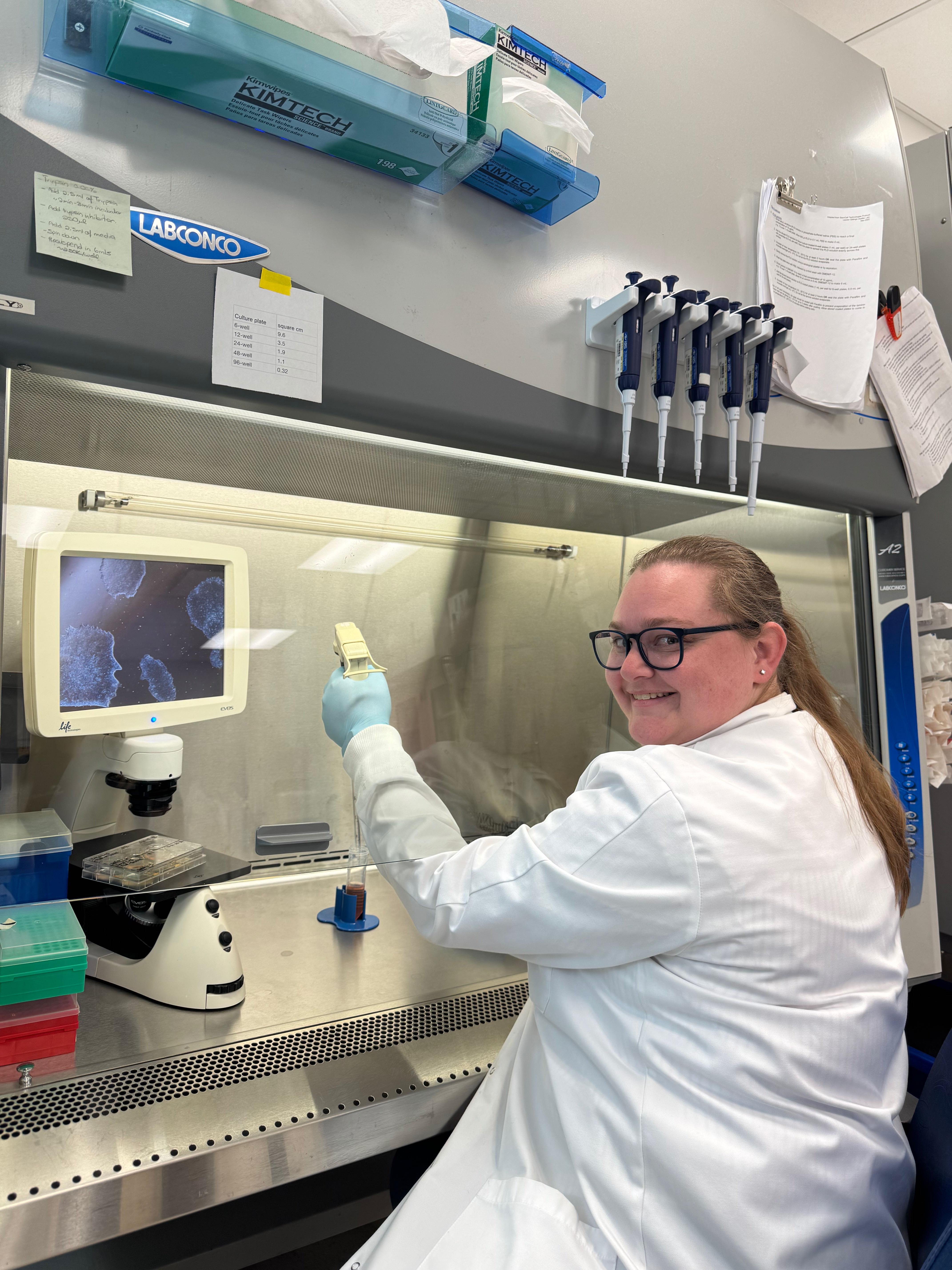
Currently, I am a PhD candidate at ASU working in the lab of Dr. Rita Sattler at Barrow Neurological Institute. With Dr. Sattler, we study the neuromuscular disorder, ALS, which sadly has an average life expectancy of 3-5years after symptom onset, and frontotemporal dementia, the most common form of dementia in individuals under the age of 60. These two diseases happen to exist on a spectrum with shared symptomatic, genetic, and pathological hallmarks. My work focuses on trying to elucidate how neuroinflammation is incited in these diseases and how it may contribute to disease onset and progression by utilizing induced pluripotent stem cells (iPSCs). These are cells which are derived from patient blood samples and allow us to better study disease by providing a human modeling system instead of animal models. iPSCs offer the unique opportunity to study the most common forms of neurodegenerative diseases which are classified as sporadic disease, meaning there is no known genetic cause. From these iPSCs, I can generate the local immune cells of the brain, known as microglia and astrocytes, and study how they interact with one another, and the cell types lost in disease, neurons. I have been fortunate to have my work and education supported by the Barrow Neurological Foundation, the Muscular Dystrophy Association, the LoBrutto Family Fund, End the Legacy, and the ARCS Foundation. Most recently, I received the highly competitive national F31 Fellowship funded through the NIH. This fellowship was awarded based on my proposal to identify neuroimmunological signatures of ALS/FTD that will hopefully lead to the discovery of novel biomarkers of disease and therapeutic targets to help diagnosis and treat this devastating disease spectrum. The recent advances in therapies for neurodegenerative disease, highlight the promising future that may be possible for patients with the continued support for scientific research like mine.
Briana Ondatje is a PhD Candidate in Neuroscience at ASU in the lab of Dr. Rita Sattler of the Barrow Neurological Institute. She is a Helen Jacobsen Pierson Scholar.